Foods with High Phosphorus Content
Meats
- Fish & seafood
- Bacon
- Beef
- Lamb
- Liver
- Turkey
- Veal
Dairy Products
- Milk
- Cheese
- Cottage cheese
- Yogurt
- Ice cream
- Pudding
Carbohydrates
- Bran cereals
- Oatmeal
- Whole grain products
Dried Beans & Peas
- Baked beans
- Black beans
- Garbanzo beans
- Kidney beans
- Lentils
- Pinto beans
- Refried beans
- Split peas
- Soy beans
Beverages
- Beer/ale
- Cocoa
- Chocolate drinks
- Dark soda
- Bottled iced tea
Nuts & Seeds
- Most nuts & seeds
- Almonds
- Cashews
- Pistachios
- Peanut butter
- Pecans
- Pumpkin seeds
- Sunflower seeds
Foods with Lower Phosphorus Content
Fresh Fruits & Vegetables
- All fruits and vegetables are low in phosphorus
Beverages
- Fruit juices
- Light colored soda
- Tea
- Coffee (no dairy)
- Home-brewed iced tea
Carbohydrates
- Breads (white)
- Crackers (not wheat)
- Pasta
- Popcorn
- Corn & rice cereal
- Rice (white)
Meat
- Fresh meat (check for added PHOS)
- Hot dog
- Sausage
- Egg
What is Phosphorus?
Phosphorus is a mineral that helps build strong, healthy bones and keeps muscles working correctly. When food containing phosphorus is consumed and digested, the small intestines absorb it and it becomes stored in the bones. Kidney disease may cause the kidneys to be unable to remove excess phosphorus from the blood.
High phosphorus levels cause bones to weaken and lead to dangerous calcium deposits in blood vessels, eyes, lungs, and heart. Levels of phosphorus in the blood should be monitored by a healthcare provider.
The normal level of phosphorus should range from 2.4 to 4.1. Low phosphorus diets limit total consumption to 800-1,000 mg daily. Check with your physician to receive the daily limit that is right for you.
Hyperphosphatemia is the medical term that describes an electrolyte disturbance in which there is an abnormally-elevated level of phosphate in the blood.
Examples of Foods That May Have Added Phosphorus:
- Frozen uncooked meats and poultry
- Frozen baked goods
- Chicken nuggets
- Cereals, cereal bars
- Baking mixes
- Instant puddings
- Sauces
Steps You Can Take to Keep Phosphorus at Safe Levels:
- Know what foods are lower in phosphorus.
- Pay close attention to serving size.
- Eat smaller portions of foods that are high in protein.
- Eat fresh fruits and vegetables.
- Ask your physician about using phosphate binders at meal time.
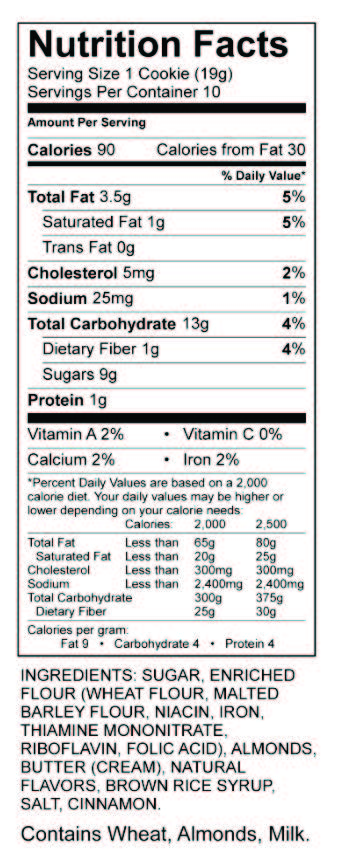
- Avoid prepackaged foods that contain added phosphorus. Look for phosphorus, or for words with PHOS, on ingredient labels, like the one below.
One Serving:
Fruit is one small piece, 1/2 cup fresh, canned or cooked fruit, or 1/2 cup juice.
Vegetables is 1/2 cup fresh or cooked vegetables, 1 cup raw leafy vegetables, or 1/2 cup juice.
Meat is 1-3 ounces cooked.
Bread is one slice.
Eggs is 1 egg or 1/4 cup egg substitute.
Rice, noodles, and pasta is 1/3 cup cooked.