
A multi-center study, led by Dr. Tobias Huber and Dr. Nicola Tomas in Hamburg, Germany, has confirmed that anti-nephrin autoantibodies (ANAAs) are commonly found circulating in the blood of patients with minimal change disease, idiopathic nephrotic syndrome and some patients with primary focal segmental glomerulosclerosis (FSGS).
This discovery relates to earlier NephCure funded ANAA research, completed by Dr. Astrid Weins, which allows us to understand the cause of some forms of rare kidney disease (RKD), develop an ANAA biomarker or lab test, and better understand which treatments may target the cause of these forms of RKD.
What is a nephrin?
Nephrin is a key protein in the kidney filter. In the kidney filters, special cells called podocytes connect with each other using finger-like processes. These connections help form an important part of the kidney filtration barrier. Nephrin helps this barrier work by talking to other molecules and sending information back to the podocyte. This helps the podocyte know how to change its shape and structure, which is important for the filtration function of the glomeruli. If nephrin doesn’t work correctly, protein and other molecules to may leak into the urine, causing a kidney condition such as nephrotic syndrome.
What are anti-nephrin autoantibodies (ANAAs)? And what effect do they have?
ANAAs are antibodies that attack nephrin proteins in the kidney filters. In this study, researchers found these antibodies in about two-thirds of adults with minimal change disease and active nephrotic syndrome before they started treatment. In children with idiopathic nephrotic syndrome, they found these antibodies in 90% of cases before treatment with steroids. A smaller number of patients with primary FSGS also had these antibodies.
In contrast, when patients were in remission or not leaking protein, these antibodies were notably reduced, or absent, which indicates ANAAs potentially play an important role in disease activity and progression.
“The discovery of anti-nephrin autoantibodies thoroughly changes our understanding of idiopathic nephrotic syndrome, minimal change disease and primary FSGS, which will now classify as anti-nephrin associated podocytopathies,” Dr. Tobias Huber stated.
“The immediate effect of the identification of anti-nephrin antibodies as specific disease markers that strongly correlate with disease activity is that we for the first time have a blood biomarker at hand, allowing to make a specific and pathobiology-based diagnosis.”
Why is this discovery so important?

This finding may change our understanding of idiopathic nephrotic syndrome, minimal change disease, and primary FSGS. These diseases are now seen as related to anti-nephrin, which helps patients understand what may be causing their illness, making the term ‘idiopathic’ (meaning unknown cause) less accurate.
Through these discoveries and studies to come, it is anticipated that anti-nephrin associated kidney disease treatment will impact patients in the following ways:
1. Improved Diagnostics
The presence of ANAAs may serve as a biomarker or diagnostic blood test that will likely provide a more accurate diagnosis. Patients who test positive for ANAAs will know a potential cause of their kidney disease and eliminate the “idiopathic” or unknown nature of their diagnosis.
2. Monitoring of Disease Activity and Treatment
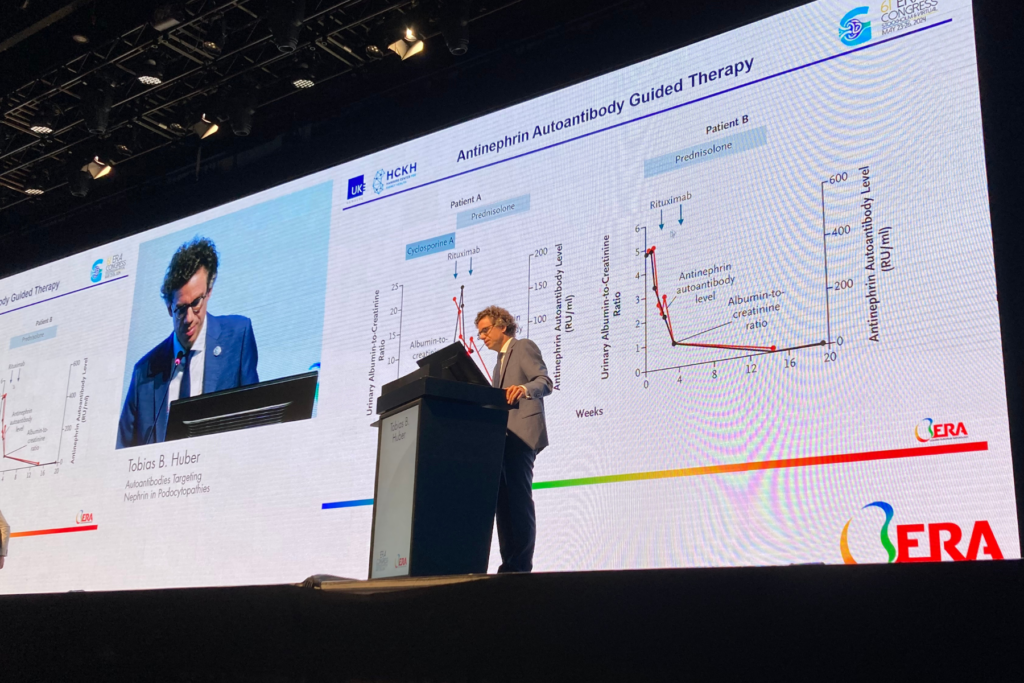
The levels of ANAAs may correlate with disease activities such as disease onset, relapse, remission, and progression. The ability to eventually monitor ANAAs in the blood may allow for real-time measurements of how patients are responding to treatment and tailored treatment strategies based on antibody levels.
3. Personalized Treatment Approaches
Current treatment protocols often involve a trial-and-error approach with steroids and non-specific immunosuppressive therapies, leaving patients with no universally accepted standard of care. Identifying patients who test positive for anti-nephrin antibodies may soon allow for more personalized treatment protocols that target specific cells, some of which are already on the market.
For patients in End Stage Kidney Disease considering a kidney transplant, measuring the amount of ANAAs could become an essential part of pre-transplant work and treatment to potentially reduce the risk of post-transplant disease recurrence.
4. New Targeted Medications
Along with medications already on the market, a deeper understanding of what factors are causing damage to the kidneys will lead to new antibody-targeted therapies, which address the underlying issues. These precision medications will also likely reduce the number negative side effects and improve outcomes compared to the use of immunosuppressive medications.
5. Deeper Understanding and New Research
There is much to learn about how ANAAs impact the kidneys. Further studies are necessary to determine if they can be used to predict a patient’s response to therapy, risk of relapse and disease course. This research study is just the beginning. It will lead to more research, a deeper understanding of both anti-nephrin mediated kidney disease and may also help in identifying other similar biomarkers for different forms of RKD.
Through continued collaboration among research consortiums and academic institutions across the world, physician and patient organizations, and people living with RKD, it’s estimated that a commercially available ANAA biomarker to inform diagnostics and disease course will be implemented within 3 years (it is currently available in only a limited number of academic research laboratories).
“The discovery of anti-nephrin antibodies as a major cause of nephrotic syndrome was the result of having the training and experience to recognize something that others did not, accepting the challenge to walk down an unbeaten path, and last but not least, assembling a team of believers that could execute and follow up with scientific rigor,” NephCure-funded researcher, Dr. Astrid Weins said.
NephCure’s contributions to research to find cures and patient advocacy continue to be the organization’s top priority. This study marks a crucial step towards revolutionizing the diagnosis and treatment landscape for some RKD patients, allowing for more clear-cut and effective management and outcomes.
“NephCure played an enormous role in all of this. Clearly, this scientific advance would not have happened without that first NephCure patient meeting I attended 20 years ago, all the research they sponsored over the years, the scientific exchange they facilitated and the resources they helped create. I owe NephCure a tremendous amount of gratitude for all this; but most importantly, for tirelessly reminding me of what it’s all about: our patients” Dr. Weins added.

How can I get involved and stay updated?
Patients can take an active role in participating in clinical trials and other longitudinal studies and registries. Helping spread the message and collecting data is
critical in finding new potential treatment options. Click here to learn more about the current RKD clinical trials taking place and see if you are eligible.
If you have specific questions regarding the ANAA discovery, please reach out to NephCure at info@nephcure.org or submit a form on our Patient Navigation services page. NephCure will continue to post updates regarding this research.
