The summer before 8th grade, I began to experience extreme fatigue. No matter how long I slept at night, I could not keep up with my friends. I often woke up with swelling in my neck, face and eyes. Sometimes I vomited for no apparent reason. My parents had been taking me to doctors for years but nobody could pinpoint the cause of my symptoms. I was tested for a variety of diseases and visited almost every unit in the children’s hospital. Finally, we landed in the Rheumatologist’s office. She told us that nothing abnormal showed up in my blood work but to come back if my symptoms grew worse or I experienced swelling in my feet or legs.
One night while I was at camp, our counselors told us to get ready to play capture the flag. I ran to put on my sneakers but no matter how hard I pushed my foot into my sneaker, it would not slip in. I looked down and realized the entire bottom half of my body, from my toes to knees, had swelled up like a balloon. The counselors and doctor on hand attributed the swelling to being out in the heat, walking around campus and eating salty foods. When I mentioned the swelling to my mom, she thought the same thing.
However, after I returned home from camp, the swelling did not disappear. In fact, it stayed exactly the same. My mom made an appointment with my Rheumatologist, who ordered blood work immediately. Two weeks later, I found myself sitting on the examination table in a Nephrologist’s office. The blood work showed I had signs of protein spillage and kidney damage. The team of doctors suspected I had Nephrotic Syndrome, a rare form of kidney disease. I could not believe this was happening. I felt as though I did not belong to my body, and instead, was watching this unfold on a movie screen. I can only describe it as an out of body experience.
I spent two days in the hospital after undergoing a kidney biopsy. The results confirmed I did in fact have a form of Nephrotic Syndrome known as Membranous Nephropathy. In everyday words, this meant I had a kidney disease and damage as a result of Lupus that went undetected for years. Lupus is an autoimmune disorder in which the body cannot tell the difference between good and bad cells. As a result, it attacks healthy tissues, such as joints and major organs.
It is difficult to describe the feelings I had while receiving this diagnosis. Part of me was confused over all the medical terminology. Part of me was sad. Part of me was overwhelmed and angry that my body had failed me. But after hearing how the doctors would treat my disease, almost all of me became scared. Along with diet and activity restrictions, I was prescribed several heavy-duty medications. Prednisone was one of the medications that would give me the most side effects. As the doctor rambled off the side effects I grew increasingly frightened. She said I would have mood swings, low energy, an upset stomach, grow “chipmunk cheeks,” and gain as much as thirty pounds – all in the course of just a few weeks after starting treatment.
I remember this like it was yesterday. After my doctor’s appointment, my mom dropped me back off at school. I did not want to show I was upset or worried, so I told her I wanted to go back to class. As I sat in my desk in the back of Mrs. LaFave’s English classroom, I stared straight ahead of me. She rambled on and on about the Masque of the Red Death and all these other Edgar Allan Poe pieces, but all I could hear was my doctor’s voice rattling off the symptoms of Prednisone. What would people think?
I was on a heavy dose of Prednisone throughout my 8th grade year. Without fail, the Prednisone showed its nasty side effects. By November, I gained about 15 pounds, was always exhausted and had round, chubby, chipmunk cheeks. As I stood in front of the mirror, I did not recognize the person staring back at me. Going to school everyday was challenging. As I walked down the hall I heard whispers. Rumors circulated about why my appearance drastically changed in such a short amount of time. “Did you have some kind of weird surgery?” random students asked me. “What’s wrong with Lauren’s face?” they would ask my friends.
I did not want to share my health problems with anyone. I was worried people would treat me differently if they knew about my disease. I did not want my teachers to feel bad for me and give me special privileges. I also wanted to appear strong for myself and my family. The last thing I wanted was my parents to worry about me.
One afternoon, I sat in the cafeteria eating lunch with three of my girl friends. I looked up and noticed the girls sitting in the next booth were staring at me. One of them leaned over and whispered something in her friend’s ear. It was clear they were gossiping about me. This was probably my breaking point. I had experienced other incidents like this before since being on Prednisone. Girls, who never cared to give me the time of day before, asked me what happened to my face. A group of kids in my math class whispered about it constantly, as if I could not hear them. When I left class every second period to go take my medicine at the nurse’s office, kids asked me why I always left class. But it was something about this one particular incident that broke me. I held in my feelings all day. By the time I walked through the door at home, I could not take it anymore. I burst into tears. My mom held me and rubbed my back as I lay in bed.
This was one of the first times in my life I felt completely shattered. It boggled my mind to think that my peers could be so critical of someone’s appearance when I had no control over it. This may seem weird to say, but during this time, I also realized I had been so blessed. My condition could have been so much worse than it actually was. I could have needed a transplant. My doctors could have put me on dialysis. I could have been admitted to the hospital for weeks instead of a few days. As I went to the hospital for my monthly checkup and blood work, I saw children who were hooked up to a million machines. Newborn babies were being poked for blood work. Children were battling cancer and fighting for their lives. I was still able to sleep in my own bed at night. I didn’t need to have different IVs pump fluids into my body. Instead, I just had to take some medicine. I could run around outside and go to a real school. My friends and I still hung out on the weekends. During this time, I was also showered by so much love and support. My parents were amazing. They made me special low-salt dinners. When I cried, they listened and wiped away my tears. My doctors went above and beyond their job description. They provided me with emotional support and hugged me after every appointment. My friends at school stood up for me when other students gossiped and spread rumors. My church family visited me in the hospital, sent cards and spoiled me with special treats.
Looking back now as an adult, I am extremely grateful for this experience. It taught me so much about myself. I learned how to be disciplined to eat healthy, get enough sleep and take my medicine on time. I learned to listen to my body and identify when it told me to slow down. As of today, I still have Lupus but my kidney disease is in remission. I am thankful everyday for a healthy body that allows me to lead a happy, normal life. It also taught me life lessons. I never judge a person based on the outside or first impressions. Everyone has a story that has shaped who they are today. Until you have walked in their shoes, it is unfair to place judgment. During the teenage years where gossip spread like wild fire, I learned just how hurtful rumors can be. I learned how important it is to be kind to everyone, regardless of how they dress, speak, or who they hang out with.
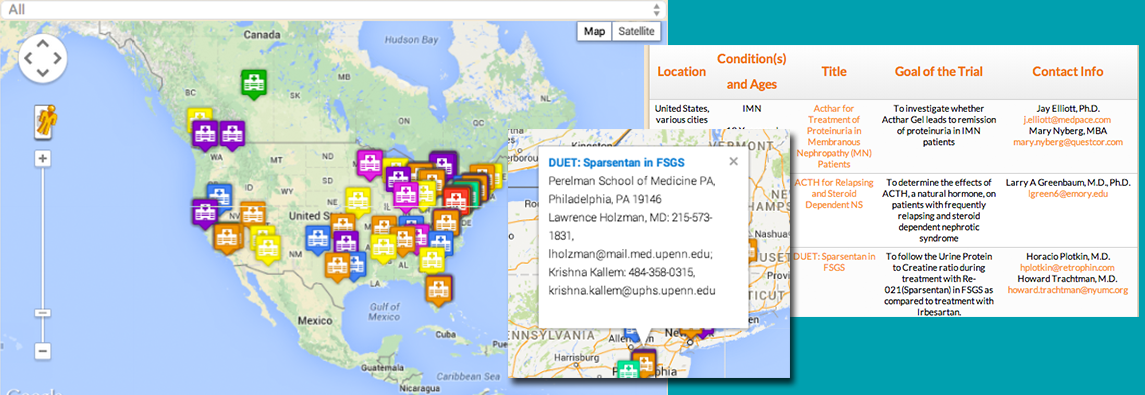
Today, I intern for NephCure Kidney International. I love interacting with patients, hearing their stories, and sharing my own personal experience with them. I realized this struggle was put in my life so I could share my story with other people.
For those who are still struggling with Nephrotic Syndrome or FSGS, there IS light at the end of the tunnel. It may not seem like it at the time, but things do get better. Those chipmunk cheeks don’t stay round forever. The kids who may be gossiping or picking on you, won’t mean a thing in a few years. Nothing is ever as bad as it may seem at the time. You will realize this experience made you a stronger person.